Diabetic Retinopathy: Protecting Your Vision from Diabetes
What Is Diabetic Retinopathy?
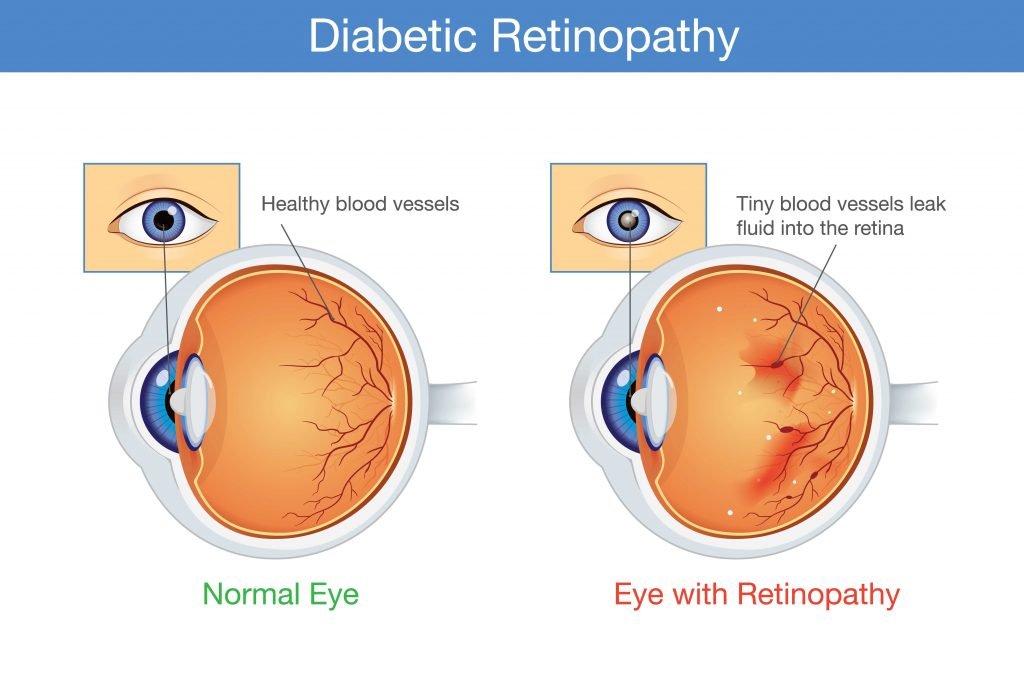
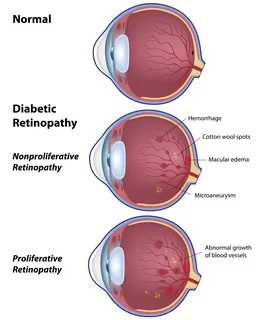
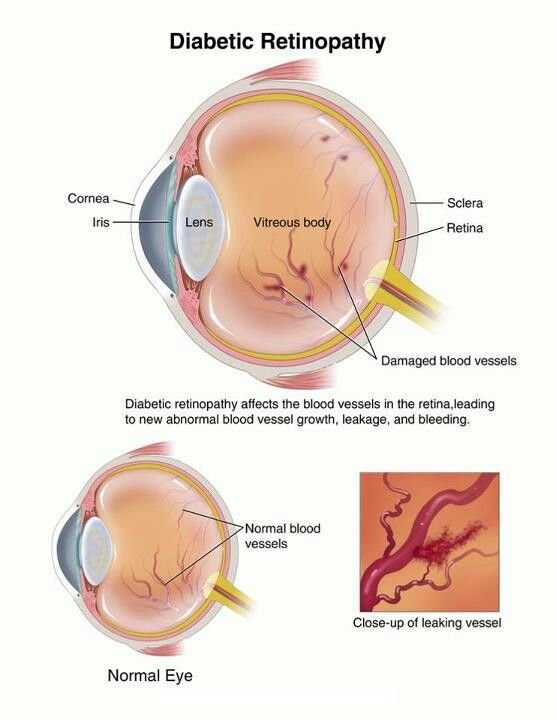
Diabetic retinopathy is a complication of diabetes that affects the eyes. It occurs when high blood sugar levels cause damage to the blood vessels in the retina—the light-sensitive tissue at the back of the eye. Over time, these damaged vessels can leak fluid or bleed, distorting vision. In advanced stages, new abnormal blood vessels may grow, leading to further vision problems.
Causes and Risk Factors
The primary cause of diabetic retinopathy is prolonged high blood sugar levels. Risk factors include:
● Duration of Diabetes: The longer you have diabetes, the higher the risk.
● Poor Blood Sugar Control: Increases the likelihood of developing retinopathy.
● High Blood Pressure and Cholesterol: Can exacerbate the condition.
● Pregnancy: Can increase the risk of diabetic retinopathy.
● Tobacco Use: Smoking can contribute to the progression of the disease.
Symptoms
Early detection through regular eye exams is crucial. Diagnostic procedures may include:
● Dilated Eye Exam: Allows the doctor to examine the retina and optic nerve for signs of damage.
● Fluorescein Angiography: Involves injecting a dye into your arm to highlight blood
● Optical Coherence Tomography (OCT): Provides detailed images of the retina’s thickness to detect swelling.University of Miami Health System+1University of Miami Health System+1 vessels in the eye.
Treatment Options
When to Seek Medical Attention
If you experience sudden vision changes, such as blurriness, spots, or flashes of light, contact an eye care professional immediately. Regular comprehensive eye exams are essential for individuals with diabetes to detect diabetic retinopathy early and prevent vision loss.